Gastroesophageal Reflux Disease (GERD)
🔹 What is GERD?
GERD occurs when stomach acid frequently flows back into the esophagus—the tube that connects the mouth to the stomach—causing irritation of the esophageal lining. Many people experience acid reflux occasionally. GERD may be mild (occurs at least twice a week) or moderate to severe (occurs once a week or more). While symptoms can often be managed with lifestyle changes, more severe cases may require stronger medications or surgery.
🔹 What are the symptoms of GERD?
- A burning sensation in the chest (heartburn), especially after eating.
- Chest pain.
- Difficulty swallowing.
- Regurgitation of food or sour liquid.
- Sore throat and a dry cough.
- Trouble sleeping due to nighttime reflux.

Important: If your GERD symptoms are severe, persistent, or you’re taking medication more than twice a week, you should schedule a consultation with Professor Dr. Tamer Saeed.
Diagnosis and Causes
🔹 How is GERD diagnosed?
- Upper endoscopy: A flexible tube with a camera examines the esophagus and stomach for inflammation.
- Acid monitoring (pH probe): A device placed in the esophagus monitors acid exposure.
- Esophageal manometry: Measures muscle contractions in the esophagus during swallowing.
- Upper GI X-ray: Uses a contrast liquid to visualize the digestive tract.

🔹 What causes GERD?
GERD results from frequent acid reflux. Normally, the lower esophageal sphincter (LES) opens to allow food into the stomach and closes afterward. If this muscle becomes weak or relaxes inappropriately, stomach acid can flow back into the esophagus, irritating and inflaming its lining.
Treatment and Surgical Solutions
🔹 Risk Factors for GERD
- Obesity
- Pregnancy
- Hiatal hernia
- Connective tissue disorders
- Smoking and alcohol
- Fatty or fried foods
🔹 How is GERD treated?
Treatment typically follows a three-step approach:
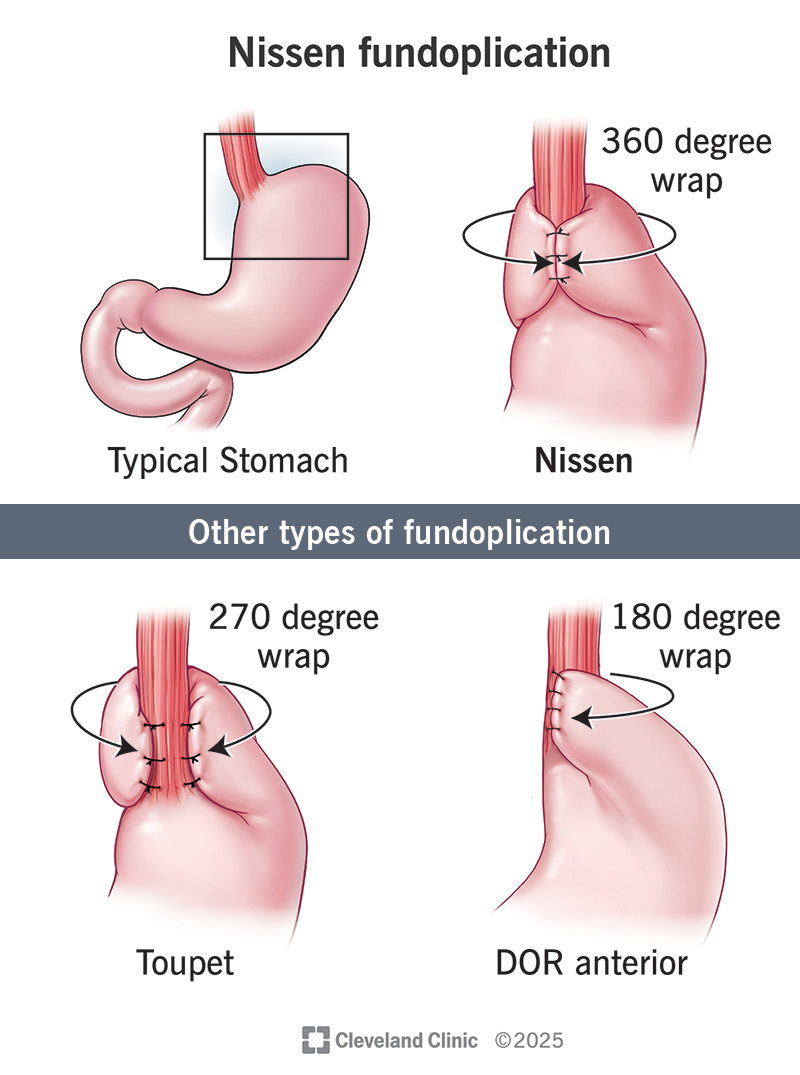
Laparoscopic Nissen Fundoplication: The Definitive Solution
This is a minimally invasive surgical procedure to permanently treat GERD by strengthening the valve between the esophagus and stomach.
⚙️ How Is It Performed?
- Done laparoscopically through 3-4 tiny incisions.
- The upper stomach (fundus) is wrapped around the lower esophagus.
- Takes about 45 minutes under general anesthesia.
✅ Why Is It Safe and Simple?
- Same-day procedure for most patients.
- Minimally invasive with less pain and quick recovery.
- Excellent outcomes and long-lasting relief.
🩺 Who Is a Candidate?
- Patients with chronic GERD not responding to medications.
- Those with severe symptoms like heartburn, chronic cough, or chest pain.
- Individuals seeking a permanent solution over long-term medication.
FAQs and Important Instructions
General FAQs about GERD
- What’s the difference between heartburn and GERD? Heartburn is a temporary symptom; GERD is a chronic disease.
- Can GERD cause shortness of breath? Yes, if acid reaches the windpipe.
- Can GERD be treated without surgery? Yes, in mild stages. Chronic cases often require surgery.
- Is the surgery painful? It is minimally invasive, and most patients return to work within a week.
- Will I need medications after surgery? Most patients do not, though some may need them temporarily.
📝 Pre-operative Instructions
- Fasting: Avoid food and drink for 6–8 hours before surgery.
- Medications: Stop certain medications (e.g., blood thinners) as instructed.
- Testing: Complete pre-operative tests (endoscopy, blood work).
- Inform Doctor: Disclose all chronic illnesses, past surgeries, and allergies.
🩺 Post-operative Instructions
- Diet: Clear liquids for 1-2 days, then soft foods. Avoid spicy/acidic foods for 4-6 weeks.
- Activity: Rest for 48 hours, then light walking. No heavy lifting for 4 weeks.
- Follow-up: Visit your doctor within a week of surgery.
- Warning Signs: Monitor for fever, severe pain, difficulty swallowing, or bleeding.
- General Advice: Sleep elevated, eat small meals, and don’t lie down for 2 hours after eating.
Diet After GERD Surgery
🚫 Foods and Drinks to Avoid (4-6 Weeks)
Acidic Foods
- Spicy foods
- Tomatoes & citrus
- Raw onions & garlic
- Chocolate & peppermint
Drinks to Avoid
- Coffee & strong tea
- Carbonated drinks
- Acidic juices
- Energy drinks
Hard-to-Digest Foods
- Fried & fatty foods
- Cabbage & broccoli
- Legumes (first month)
- Heavy desserts
✅ Recommended Foods
Introduce gradually; start with soft or mashed foods.
Liquids
- Water
- Strained soup
- Low-fat dairy
- Herbal teas
Soft Foods
- Mashed potatoes
- Rice & pasta
- Steamed vegetables
- Grilled chicken/fish
Fruits
- Cooked apple
- Banana
- Ripe pear
- Melon
Light Protein
- Egg whites
- Cottage cheese
- Water-packed tuna
Contact Us
For appointments and inquiries about GERD treatment and the latest surgical techniques.
Location: Saudi German Hospital, Dubai, UAE
Phone: +971-58-675-8981