A Guide to Bariatric Surgery
Comprehensive Information on Obesity and Its Treatments
What is Obesity?
Obesity is a condition characterized by a decreased rate of fat metabolism, leading to fat accumulation in the body and consequently weight gain.
How is Obesity Measured?
The most accurate method for determining the degree of obesity is the Body Mass Index (BMI) calculation, which is derived by dividing a person’s weight in kilograms by twice their height in meters:
BMI = Weight (kg) / [2 × Height (m)]

BMI Classification:
- Less than 25: Normal weight
- 25 to 30: Overweight
- 30 to 35: Obesity Class I
- 35 to 40: Obesity Class II
- More than 40: Morbid or Severe Obesity, which often requires surgical intervention
What is Morbid Obesity?
Morbid or severe obesity is defined as having a BMI greater than 40.
What are the Causes of Obesity?
Obesity can result from a variety of factors, including genetic predisposition and certain medical conditions such as hypothyroidism or elevated cortisol levels. However, the most common causes are unhealthy lifestyle habits—such as a reliance on fast food, consumption of sugary sodas, and lack of physical activity—which disrupt the balance between calorie intake and calorie expenditure.
What Are the Health Risks Associated with Morbid Obesity?
Morbid obesity is strongly linked to several serious health problems, including:
- Type 2 diabetes
- Cardiovascular diseases such as hypertension, high cholesterol, and heart rhythm disorders
- Increased risk of blood clots, particularly in the lungs and legs
- Joint inflammation
- Gastroesophageal reflux disease (GERD)
- Obstructive sleep apnea
-
Infertility and reproductive issues, such as:
- Polycystic ovary syndrome (PCOS)
- Irregular menstrual cycles in women
- Low sperm count and erectile dysfunction in men
Additionally, obesity is associated with a higher risk of certain cancers, including colon, breast, and uterine cancer.
Is There a Link Between Obesity and Mental Health?
Yes. Studies have shown that individuals with obesity are more prone to depression due to feelings of helplessness, limited mobility, social isolation, and the psychological burden of obesity-related health issues, such as infertility.

What Are the Treatment Options for Obesity?
Treatment may be medical and psychological, primarily focusing on lifestyle modification, including adopting a healthy diet and, in some cases, using medications that promote fat burning.
Alternatively, surgical treatment is often the most effective option for cases of morbid obesity, especially when other methods have failed. However, surgical treatment must be accompanied by long-term lifestyle changes and strict adherence to nutritional guidelines to ensure success.
What Are Bariatric Surgeries and How Do They Work?
Bariatric surgeries are procedures designed to help patients lose weight and reach a healthy body weight. These surgeries are generally categorized into two main types:
- Restrictive procedures, which reduce the size of the stomach and thereby limit food intake. Examples include gastric sleeve, gastric band, and gastric balloon. This type of surgery is ideal for patients who consume large portions of food.
- Malabsorptive-restrictive procedures, which both reduce the size of the stomach and bypass a portion of the small intestine responsible for absorbing fats and sugars. Examples include gastric bypass procedures. These are best suited for patients who consume large quantities of sweets and high-calorie foods.
Eligibility and Choosing Your Surgeon
Who Needs Bariatric Surgery?
Bariatric surgery is recommended for patients who meet one of the following criteria:
- Morbid obesity, defined as a Body Mass Index (BMI) over 40.
- A BMI over 35 with obesity-related health problems such as type 2 diabetes, high blood pressure, high cholesterol, polycystic ovary syndrome (PCOS), or infertility.
Note: Morbid obesity can also be defined as a weight exceeding the normal weight by 40 kilograms in men or 35 kilograms in women.
How to Choose a Bariatric Surgeon?
What qualifications should a bariatric surgeon have?
- A doctoral degree in General and Gastrointestinal Surgery.
-
Significant experience in bariatric surgery, demonstrated by:
- Working within a specialized bariatric surgery team or department.
- Performing over 1500 bariatric surgeries.
- Active participation in international bariatric surgery conferences.
- Publishing research in international medical journals.
Stages of Bariatric Surgery
1. Preoperative Stage
This stage is one of the most critical for the success of bariatric surgery. It includes:
- Accurate diagnosis of the cause of obesity and ruling out underlying medical conditions.
- Selecting the most appropriate surgical technique and thoroughly explaining the procedure.
- Managing comorbidities such as diabetes or hypertension.
- Increasing protein intake to promote healing and reduce the risk of complications like leakage.
2. Intraoperative Stage
This is the most delicate stage and requires high attention to detail. Key considerations include:
- Choosing a top-tier hospital equipped with advanced intensive care units.
- Using high-quality surgical tools and premium consumables from reputable brands.
- Employing the latest vessel-sealing technologies.
- Ensuring the presence of a highly experienced surgical team.
3. Postoperative Stage
This stage is equally important and involves:
- Close monitoring during the first few days after surgery to detect and manage any complications early.
- Follow-up over the first two years to monitor weight loss progress and nutritional adequacy.
- Offering post-weight loss body contouring services to help patients achieve their ideal body shape.
Preoperative Instructions
1. Psychological Preparation and Commitment
- You must be mentally prepared to make permanent lifestyle changes.
- Strict adherence to dietary guidelines and physical activity after surgery is essential for long-term success.
2. Required Medical Examinations
- You will undergo comprehensive blood tests, abdominal imaging, and assessments of heart and lung function.
- Consultation with a nutritionist and psychologist may be required.
3. Preoperative Diet
- Follow a low-calorie diet for 1–2 weeks before surgery.
- Avoid heavy meals for at least 12 hours before surgery.
- No food or drink for 8 hours prior to the procedure.
4. Smoking and Medication Cessation
- Stop smoking at least two weeks before surgery.
- Discontinue blood thinners and aspirin as per your doctor’s instructions.
5. Management of Chronic Medications
- Inform your surgeon of all your regular medications.
- Do not stop any medication without consulting your doctor.
Postoperative Instructions
1. Hospital Stay and Monitoring
- Expect to stay in the hospital for 1–2 days for observation.
- A catheter or temporary drainage tube may be placed.
2. Post-Surgery Diet Plan
- Week 1: Clear fluids only.
- Week 2: Full fluids.
- Weeks 3–4: Pureed and soft foods.
- Second Month: Gradual reintroduction of solid foods.
3. Activity and Movement
- Walking is encouraged from day one to prevent blood clots.
- Avoid heavy lifting or strenuous exercise for 4–6 weeks.
4. Medications and Supplements
- Take prescribed painkillers and antibiotics as directed.
- Lifelong adherence to vitamin and mineral supplements is necessary.
5. Medical Follow-up
- Regular check-ups with your surgeon and dietitian.
- Periodic monitoring of weight, vitamin levels, and blood tests.
6. Warnings
Contact your doctor immediately if you experience severe pain, high fever, persistent vomiting, or swelling around the surgical site.
A Detailed Guide to Bariatric Procedures
In-depth Information on Specific Surgeries

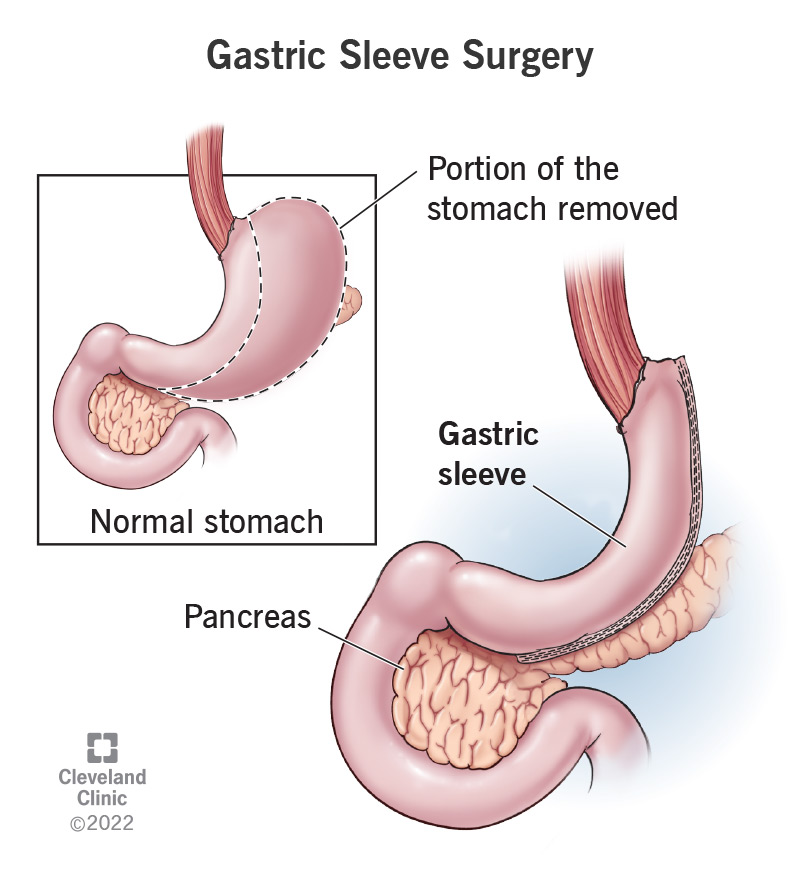
Gastric Sleeve Surgery (Sleeve Gastrectomy)
What is Sleeve Gastrectomy?
It is a surgical procedure that reduces the size of the stomach by removing a large portion, leaving behind a narrow tube-shaped stomach of approximately 100 ml in capacity.
It is one of the most popular and effective bariatric procedures today and is the first choice in many countries.
How Does It Work?
The procedure works by:
- Reducing stomach volume, limiting food intake.
- Removing the part of the stomach that secretes hunger hormones, resulting in reduced appetite and early satiety.
Weight Loss Outcomes
- Patients typically lose 50% of their excess weight within 6 months.
- Most return to normal weight within one year after surgery.
Improvement in Diabetes and Other Conditions
- 60% reduction in blood sugar levels within 6 months.
- 85% of patients experience complete resolution of type 2 diabetes within one year.
Recovery Timeline
- Hospital discharge usually occurs 2 days after surgery.
- Return to normal activities and work is expected within 10 days.
Vitamin Deficiency After Surgery
- Since the food follows the natural digestive pathway, patients rarely experience deficiencies in vitamins or minerals.
- Therefore, hair loss and brittle nails are uncommon.
Disadvantages of Sleeve Gastrectomy
- The removed portion of the stomach cannot be restored.
- The stomach may stretch over time if dietary guidelines are not followed.
- Not suitable for patients who frequently consume sweets, chocolate, ice cream, or carbonated beverages.
FAQs & Considerations
Who Is a Candidate for Sleeve Gastrectomy?
- Patients with obesity due to consuming large quantities of food in one sitting.
- BMI of 40 or more, or 35 or more with associated health issues like diabetes, hypertension, PCOS, or infertility in men and women.
Can Patients Get Pregnant After Surgery?
Yes, pregnancy is allowed after surgery as long as all vital nutrients and biochemical parameters are within normal levels.
Causes of Stomach Stretching After Surgery
- Eating beyond the feeling of fullness.
- Drinking water during meals.
- Consuming carbonated beverages.
How to Prevent Stomach Stretching
- Avoid eating until completely full.
- Refrain from drinking during meals.
- Avoid all carbonated drinks.
Possible Complications
- Staple line leak or gastric perforation, usually due to delayed healing. Often treated with endoscopic stents or clips.
- Abdominal fluid or blood collection, especially during the first week due to internal bleeding. May require re-exploration and drainage.
- Fatigue and nausea during the first 2–4 weeks as the body adapts to the new diet.
- Hair loss and brittle nails, rarely occurring, often related to vitamin B6 deficiency, and manageable with increased protein and vitamin intake.
What Causes Vitamin Deficiency After Sleeve Gastrectomy?
- Poor patient preparation with pre-existing deficiencies not diagnosed or treated before surgery.
- Poor postoperative nutrition choices.
Both are easily treatable with the right dietary sources and nutritional planning.
Contraindications for Sleeve Gastrectomy
- Presence of gastric ulcers or severe GERD (reflux disease).
- Inability to stop binge eating sugary foods.
Gastric Bypass Surgery
What is Gastric Bypass Surgery?
Gastric bypass is a surgical procedure that involves reducing the size of the stomach and connecting it directly to the lower part of the small intestine. This limits both food intake and nutrient absorption.
Types of Gastric Bypass
1. Classic Gastric Bypass (Roux-en-Y)
Involves two connections (anastomoses): one between the stomach and the intestine, and another between two parts of the intestine.
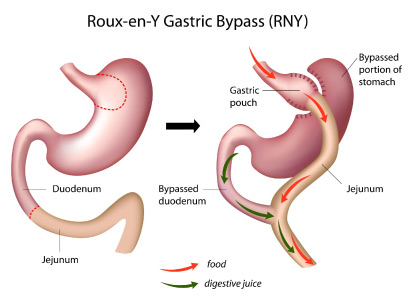
2. Mini Gastric Bypass
Involves only one connection between the stomach and the intestine, making it simpler and faster.

How Does the Surgery Work?
Gastric bypass works through two mechanisms:
- Restriction: Reduces stomach size, resulting in early satiety with smaller meals.
- Malabsorption: Bypasses the upper part of the small intestine responsible for absorbing fats and sugars, reducing calorie absorption.
Who is a Candidate for Gastric Bypass?
This procedure is suitable for:
- Patients with a BMI over 40, especially those with a high intake of sugary foods.
- Patients with a BMI over 35 who suffer from obesity-related diseases such as diabetes, hypertension, or high cholesterol.
Complications of Gastric Bypass Surgery
- Vitamin Deficiencies and Anemia: Due to malabsorption, patients may develop deficiencies in essential nutrients leading to hair loss and fatigue. Lifelong supplementation is required.
- Digestive Disturbances: Some patients experience bloating, indigestion, or irritable bowel symptoms. These can be managed with medications.
- Excessive Weight Loss: In rare cases, patients may lose too much weight and require reversal or revision surgery.
- Leaks at the Surgical Connection: Although rare, leaks at the stomach-intestine junction can occur and may require surgical intervention.
Weight Loss After Gastric Bypass
Patients typically lose about 70% of their excess weight within 8 months and achieve their ideal weight within one year.
Improvement in Obesity-Related Conditions
Gastric bypass is one of the most effective procedures for resolving comorbidities:
- Studies show 95% of type 2 diabetes cases are resolved within one year.
- Also improves hypertension and cholesterol levels significantly.
How Does Gastric Bypass Affect Diabetes?
The procedure improves diabetes through:
- Reduced absorption of fats and sugars.
- Reduced secretion of harmful gut hormones that interfere with insulin, thereby improving pancreatic function and enhancing insulin sensitivity.
Success Factors for Diabetes Treatment
Best results are seen in patients who still have remaining insulin production or functional pancreatic reserves before surgery.
Is It Suitable for Diabetic Patients Without Obesity?
Yes. According to several studies (including ones overseen by Dr. Tamer Saeed), modified versions of gastric bypass have shown great effectiveness in non-obese type 2 diabetics, with minimal impact on weight but high efficacy in blood sugar control.
Can Patients Get Pregnant After Surgery?
Pregnancy is not contraindicated, but it is recommended to wait at least 2 years post-surgery to ensure nutritional stability.
Complications of Gastric Bypass Surgery
-
Vitamin Deficiencies and Anemia:
Due to malabsorption, patients may develop deficiencies in essential nutrients leading to hair loss and fatigue. Lifelong supplementation is required.
-
Digestive Disturbances:
Some patients experience bloating, indigestion, or irritable bowel symptoms due to the altered digestive tract. These can be managed with medications.
-
Excessive Weight Loss:
In rare cases, patients may lose too much weight and require reversal or revision surgery.
-
Leaks at the Surgical Connection:
Although rare, leaks at the stomach-intestine junction can occur and may require surgical intervention.
Why Does Vitamin Deficiency Occur After Bypass?
It results from reduced nutrient absorption in the bypassed part of the intestine. Treatment includes improving diet quality and using vitamin-rich foods and supplements.
A Guide to Modern Bariatric Procedures
The SASI Procedure
What is SASI?
SASI stands for Single Anastomosis Sleeve Ileal Bypass. It combines a sleeve gastrectomy with a mini gastric bypass to treat obesity and type 2 diabetes.

How Does SASI Work?
- Sleeve Gastrectomy: Removes hunger hormone-producing portion of stomach.
- Bypass: Food is rerouted to the lower intestine, reducing sugar and fat absorption.
Weight Loss Results
Patients lose ~60% of excess weight in 6 months; ideal weight often reached within a year.
Improves Comorbidities
SASI improves diabetes, hypertension, and high cholesterol in 90% of cases.
Lower Risk of Deficiencies
Only ~20% experience temporary deficiencies. Most of the digestive path is preserved.
Advantages
- Combines restriction and malabsorption
- Lower complication rate
- Fewer vitamin deficiencies
Candidate Criteria
- BMI ≥ 35, especially with sugar cravings
- BMI ≥ 30 with diabetes or hypertension
The SADI Procedure
What is SADI?
SADI stands for Single Anastomosis Duodenal-Ileal Bypass. It includes a sleeve gastrectomy and a single bypass between the duodenum and a lower section of the ileum.
It’s a powerful option for patients with type 2 diabetes, especially if previous surgeries were ineffective.
Bariatric Surgery & Diabetes
Impact on Type 2 Diabetes
All bariatric surgeries improve type 2 diabetes, but results vary:
- Sleeve Gastrectomy: ~85% remission rate
- Gastric Bypass: Up to 95% remission rate
Post-Surgery & Lifestyle Guide
Managing Diabetes, Diet, and Other Considerations After Bariatric Surgery
Bariatric Surgery & Diabetes
How Do Bariatric Surgeries Help Treat Diabetes?
These surgeries act on two main mechanisms:
- Weight loss and reduced absorption of sugars and fats.
- Hormonal changes that reduce the secretion of harmful hormones affecting the pancreas, thereby improving insulin effectiveness.
Can These Surgeries Help Diabetic Patients Without Obesity?
Yes. Recent studies confirm the effectiveness of modified bariatric surgeries in treating diabetes even in non-obese patients, provided the surgical technique is adjusted to prevent excessive weight loss.
What’s New in Bariatric Surgery for Diabetes?
Newer procedures like SASI (Single Anastomosis Sleeve Ileal Bypass) have shown remarkable results in improving metabolic conditions, particularly type 2 diabetes.
What Factors Predict Better Outcomes for Diabetic Patients After Surgery?
Patients who:
- Use oral medications or
- Have used insulin for less than 10 years
respond best to surgery, as their pancreas still retains sufficient insulin-producing capacity.
Redo Bariatric Surgery
Which Bariatric Surgery Has the Highest Failure Rate?
All bariatric surgeries have a potential for failure, depending largely on the patient’s adherence to postoperative guidelines and the type of surgery performed.
Why Do Bariatric Surgeries Fail?
- Non-compliance with the dietary plan
- High intake of sweets and carbonated drinks
- Surgical technique or inappropriate choice of procedure
How Is Weight Regain Managed After Bariatric Surgery?
- If weight regain is due to behavioral issues, psychological counseling is recommended.
- If due to a technical or physiological failure, a revision surgery may be necessary.
What Is the Best Revision Surgery?
This depends on the cause of the original failure and the patient’s current condition. All bariatric surgeries can be revised if needed, and gastric bypass is generally considered the most successful and widely used revision option.
Expected Outcomes After Revision Surgery
On average, patients lose 20% less weight after a revision than they did after the first procedure due to the body’s adaptation and scar tissue.
Disadvantages of Revision Surgery
- Reduced effectiveness (10–20% less than the original surgery).
- Higher risk of complications, such as bleeding and leakage, due to adhesions and scar tissue.
Gastric Balloon
What Is a Gastric Balloon?
A gastric balloon is a non-surgical weight loss procedure in which a balloon is inserted into the stomach via an endoscope through the mouth.
How Does It Work?
The balloon fills space in the stomach, making the patient feel full after eating small portions.
How Much Weight Can Be Lost?
Patients typically lose 15–25 kilograms during the 6-month period the balloon is in place.
What Are the Success Factors for Gastric Balloon Therapy?
- Strong willpower and commitment to the prescribed diet are crucial.
- The balloon helps the patient adapt to a new lifestyle, but the stomach does not change in size permanently, so habits must change to maintain results.
Disadvantages of Gastric Balloon
- Weight regain is likely if the patient does not follow dietary instructions after removal.
- Balloon rupture may occur if left in the body for more than 6 months. In this case, urine may turn blue or red, and the balloon should be removed immediately.
- Nausea and vomiting, especially in the first week, usually resolve with medication.
- Gastric ulcers and inflammation, which may require intensive medical treatment.
When Should the Balloon Be Removed?
The balloon is typically removed 6 months after insertion.
Who Should Consider a Gastric Balloon?
- Patients who prefer non-surgical options.
- Those who have medical contraindications for surgery.
- Individuals seeking moderate weight loss, such as postpartum weight gain.
General Information on Obesity Surgeries
What You Need to Know About Mounjaro and Ozempic
In recent years, anti-obesity medications have become one of the most modern tools in weight management, especially for individuals who either prefer to avoid surgery or are not suitable candidates for surgical intervention. Among the most prominent options are Mounjaro (Tirzepatide) and Ozempic (Semaglutide).
🔹 What Are Mounjaro and Ozempic?
- Ozempic is primarily used to treat type 2 diabetes and works as a GLP-1 receptor agonist. It reduces appetite, slows gastric emptying, and improves blood sugar control, which leads to significant weight loss.
- Mounjaro is a newer medication containing Tirzepatide, which acts on both GLP-1 and GIP receptors. It has demonstrated superior weight loss results compared to Ozempic and, while currently approved for diabetes, it is sometimes prescribed off-label for obesity.
🔹 How Do These Medications Work?
- They mimic natural gut hormones that regulate hunger and fullness.
- They reduce appetite and increase the feeling of satiety.
- They improve metabolic markers like blood glucose, cholesterol, and inflammation.
🔹 Effectiveness in Weight Loss
- Ozempic can result in 10–15% total body weight loss within 6–12 months.
- Mounjaro has shown even greater effectiveness, with some studies reporting up to 20% weight loss.
- Maximum effectiveness is achieved when combined with a healthy diet and physical activity.
🔹 Who Can Benefit from These Medications?
- Individuals with obesity (BMI ≥30) or overweight (BMI ≥27) with obesity-related health conditions like diabetes, hypertension, or sleep apnea.
- Patients who have failed to lose weight through diet and exercise alone.
🔹 Side Effects and Risks
Common side effects:
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Abdominal discomfort
Rare but serious risks:
- Pancreatitis
- Gallbladder disease
- Potential thyroid tumors
- Worsening of diabetic retinopathy
Contraindications:
- Personal or family history of medullary thyroid carcinoma
- History of pancreatitis
- Severe gastrointestinal disorders
🔹 Important Notes
- These medications are administered as once-weekly subcutaneous injections.
- They are relatively expensive, and insurance coverage may vary.
- They require long-term use to maintain results.
- Abrupt discontinuation often leads to weight regain.
🔹 Conclusion
Mounjaro and Ozempic represent a major advancement in obesity treatment and can be life-changing when used appropriately. However, they are not a substitute for lifestyle changes and must be used under full medical supervision as part of a comprehensive weight management plan.
Health & Wellness Guide
Information on Bariatric Surgery, Diet, and Lifestyle
Can You Fast After Bariatric Surgery?
Fasting is not recommended during the first 6 months post-surgery.
After that, it is permitted as long as the patient has progressed to pureed foods and can drink at least 2 liters of fluids daily.
If fasting leads to fatigue, dizziness, or dehydration, the patient should break the fast.
Is There a Difference Between Fasting After Sleeve vs. Bypass Surgery?
Yes.
-
Bypass patients often experience dizziness or shakiness after eating, especially after sugary meals, due to dumping syndrome.
→These patients should avoid carbohydrates and sugars at Iftar and focus on hydration.
- Sleeve gastrectomy patients usually do not experience these symptoms and can fast more comfortably.
General Tips for Bariatric Patients During Ramadan
- Avoid exercising while fasting to prevent low blood sugar and dehydration.
- Drink at least 2 liters of fluids per day, but avoid drinking while eating.
- Reduce intake of sugar and salt.
- Break the fast with warm fluids and dates, along with acid-reducing medications and vitamin supplements. Wait one hour, then eat small, healthy meals.
How to Reduce the Appearance of Cellulite
- Weight loss and regular physical activity are key factors.
- Drink plenty of water, avoid coffee, tea, and smoking.
- Cold showers have been shown to help improve skin tone and reduce cellulite.
Importance of Colon Preparation in Weight Loss Success
The digestive tract begins at the mouth and ends at the anus, with the colon playing a vital role in nutrient absorption.
Any inflammation or dysfunction in the colon can lead to poor fat metabolism, food fermentation, weight gain, and difficulty losing weight.
Foods That Boost Fat Burning
- Drink at least 2 liters of water daily.
- Natural boosters: ginger, parsley, green tea, cumin, mint.
- Unsweetened fruit cocktails: lemon, orange, mandarin, kiwi, pineapple.
- Vegetable blends: carrot, tomato, arugula juice.
- Cabbage juice or broth.
- Walking for 10 minutes daily can triple the metabolic rate.
Importance of Vitamin and Mineral Storage Before Bariatric Surgery
The human body requires many essential vitamins and minerals like sodium, potassium, magnesium, and vitamins A, B, C, D, E.
Rapid weight loss after bariatric surgery can lead to deficiencies.
Storing sufficient amounts before surgery and working with a clinical nutritionist helps prevent these deficiencies through tailored diets and medical supplements.
Cellulite & Skin Tightening After Weight Loss
- Exercise and cold showers are key to improving skin firmness and reducing cellulite.
- Adequate hydration and avoiding caffeine and smoking are also helpful.
- Devices like radiofrequency and lipolaser have shown effectiveness in 6–8 sessions, improving collagen production and skin tone.
Sexual Health After Bariatric Surgery
Generally, sexual performance improves after weight loss due to improved mobility and the removal of physical barriers like abdominal fat.
Many men also report enhanced sexual function and confidence post-surgery.
How to Overcome Fast Food Addiction
- Be patient—breaking this habit takes 4–6 weeks.
- Keep meals simple; overcomplicating healthy recipes can make you revert to fast food.
- Gradually reduce consumption; you don’t have to quit all at once.
- Make healthy versions of fast food at home (e.g., burgers, pizza).
- Keep a daily journal tracking your progress and challenges.
- Know the risks: fast food increases the risk of asthma, hormonal imbalances, and obesity-related conditions.
- Obese individuals are more likely to consume fast food, increasing the risk of type 2 diabetes, high blood pressure, PCOS.
-
Top 3 belly-fat-causing foods:
- Sugary drinks
- Excessive carbs
- Overconsumption of dairy (despite its calcium content)
Best methods to reduce belly fat:
- Eat fiber-rich foods
- Exercise outdoors
- Track your caloric intake
- Do abdominal and breathing exercises early in the morning on an empty stomach
Understanding Surgical Leaks
What Is a Leak After Bariatric Surgery?
A leak is when stomach fluids escape into the abdominal cavity, typically due to poor healing of the stapled area.
Leak Incidence Rate
Occurs in 1% to 3% of cases globally, often due to tissue rejection of staples.
Symptoms of a Leak
Fever, elevated heart rate, sharp abdominal pain—classic signs of leakage and possible sepsis.
How to Diagnose a Leak
Through contrast X-rays or multi-slice CT scans with oral contrast.
When Do Leaks Occur?
Most commonly between day 4 and two weeks post-op, during the stomach’s healing phase.
Causes of Leaks
- Primary cause: rejection of staples (1–3% of cases)
- Other causes: Low protein levels due to poor pre-op nutrition; use of low-quality or reused staplers.
How Are Leaks Treated?
Thanks to medical advancements, leaks are now more treatable, especially when detected early:
- If leakage is less than 100 ml/day, it can be managed medically by stopping oral intake.
- If leakage is over 1000 ml/day, endoscopic stent placement is often required.
- In some cases, surgical repair may be necessary.
Leak Prevention Tips
- Proper preoperative patient preparation, especially correcting low protein levels.
- Use of high-quality, internationally approved staplers.
- Close postoperative monitoring for early detection and management.
General Tips for a Healthy Lifestyle
Key Guidelines for Effective Weight Loss
- Successful weight loss depends on balanced eating habits, understanding your daily caloric needs, and maintaining regular physical activity.
- The best way to organize daily meals is to split food intake into 3 main meals and 2 healthy snacks.
- Eating only one or two meals per day actually reduces your metabolic rate and slows fat burning, making weight loss harder.
- Avoid eating within 2 hours before bedtime as the body digests food less efficiently during sleep.
- Avoid processed sweets and replace them with moderate portions of fruit for better adherence to a healthy diet.
- Excessive consumption of carbonated drinks, even sugar-free, and sweetened juices leads to weight gain. Choose fresh juices without sugar.
- Fresh vegetables are essential due to their high vitamin content, low calories, and beneficial fiber.
Mindset and Motivation
- Past weight loss failures do not define your future—a new beginning starts at the point you left off.
- Determination and adherence to your doctor’s instructions are key to success. Stay consistent—you deserve to live a healthy life.
A Comprehensive Guide to Dieting & Weight Loss
The complete, unabridged recommendations for your health journey.
Recommended Foods During Dieting
- Eggs are rich in protein and essential nutrients, making them ideal during dieting.
- Oats are excellent for breakfast—they’re high in fiber, promote digestion, provide satiety, and contain carbs that boost metabolism.
- Green tea activates metabolism, burns fat, and contains antioxidants. Drink 5–6 cups daily.
- While desserts are usually avoided during dieting, dark chocolate in small amounts may reduce cravings and boost fat burning.
- Cutting out carbonated drinks can help you lose nearly 1 kg per week if you normally drink 2 cans a day.
- Simple changes—like using smaller plates, teaspoons, and eating slowly (one bite every 5–10 minutes)—can reduce food intake by 25–30%.
The Role of Sleep in Weight Loss
- Sleeping 6–7 hours at night is critical. Lack of sleep disrupts hunger hormones, increasing appetite.
Breakfast and Meal Timing
- Never skip breakfast—metabolism is highest in the morning, and it helps regulate appetite throughout the day.
- Avoid feeling full after meals to prevent stomach stretching post-surgery.
- Bariatric surgery alone is not enough. To achieve results, patients must follow a structured, healthy diet.
Hydration and Meal Distribution
- Drink 1.5–2 liters of fluids daily, especially 30 minutes before meals. Avoid drinking during meals.
- Split meals into three main meals and snacks every 2–3 hours to maintain a steady metabolic rate.
Protein and Daily Activity
- Focus on fish and poultry proteins while limiting red meat due to higher fat and carb content.
- Walk for at least 15 minutes daily to accelerate fat loss.
Weight Plateau After Surgery
- Weight may plateau one month post-op due to metabolic adjustment. Don’t panic—adjustments from your nutritionist can reignite progress.
Pre-Surgery Preparation
- Follow a healthy diet for at least one week before surgery to prepare your body.
- Avoid tea, coffee, and smoking pre-surgery.
- Focus on protein, vegetables, and fresh fruits before surgery.
Exercise and Physical Activity
- If your job keeps you physically active but you’re still overweight, know that daily movement ≠ exercise. You still need dedicated workout time alongside a proper diet.
- Exercise options vary from walking, running, and swimming to aerobics and Zumba, which are highly effective when paired with diet.
- Aim to drink at least 3 liters of fluids daily, such as water or unsweetened fresh juices.
- Avoid eating in front of TV or mobile devices, as distraction leads to overeating and loss of control.
Body Shaping and Fat Redistribution
- To reshape your body during weight loss, engage in aerobics or Zumba alongside your diet.
- Excessive intake of stimulants (coffee/tea), even unsweetened, may negatively affect weight loss.
- Maintaining 6–8 hours of consistent sleep daily helps regulate metabolism and supports weight loss.
Foods to Avoid and Portion Control Tips
- Avoid high-calorie fruits like mango, dates, figs, and grapes.
- Avoid roasted nuts, as they are calorie-dense.
- During Ramadan, meals are reduced to 2 main meals and 1 snack. Prioritize unsweetened fluids, begin Iftar with a warm drink, wait 15 minutes, then have your meal.